Synergy or Challenge? Navigating Semaglutide and the Keto Diet for Optimal Health and Weight Loss
In the evolving landscape of health and wellness, two powerful tools have garnered significant attention for their potential in weight management and metabolic improvement: Semaglutide and the Ketogenic Diet. Separately, they represent distinct approaches to influencing the body’s metabolism, blood sugar, and fat burning processes. Semaglutide, a revolutionary medication, has transformed the treatment of Type 2 Diabetes and chronic weight management. The Ketogenic Diet, a long-standing nutritional strategy, promotes a metabolic state where the body burns fat for fuel.
As individuals seek increasingly effective ways to achieve their health goals, the question naturally arises: what happens when these two potent strategies are combined? Is it a synergistic path to unparalleled results, or does it present a complex array of challenges that require careful navigation? This comprehensive article delves deep into the mechanisms, benefits, risks, and crucial considerations for anyone contemplating the combination of Semaglutide and the Keto Diet. Our aim is to provide an E-E-A-T compliant guide, offering expert insights and trustworthy information to help you make informed decisions in consultation with your healthcare provider.
Understanding Semaglutide: A Game Changer in Metabolic Health
Semaglutide is a medication that belongs to a class of drugs called GLP-1 receptor agonists. It mimics the action of glucagon-like peptide-1 (GLP-1), a natural hormone produced in the gut that plays a vital role in regulating blood sugar and appetite. Approved under brand names like Ozempic (primarily for Type 2 Diabetes) and Wegovy (specifically for chronic weight management), Semaglutide has emerged as a significant breakthrough.
Mechanism of Action: How Semaglutide Works
Semaglutide’s effectiveness stems from its multifaceted impact on the body:
- Blood Sugar Regulation: When blood sugar levels rise, Semaglutide stimulates the pancreas to release more insulin. Simultaneously, it reduces the amount of glucagon, a hormone that raises blood sugar. This dual action helps to stabilize glucose levels, making it highly effective for individuals with Type 2 Diabetes.
- Slowing Gastric Emptying: Semaglutide significantly slows down the rate at which food leaves the stomach. This leads to a prolonged feeling of fullness, reducing overall food intake and subsequently aiding in weight loss.
- Appetite Suppression: By acting on receptors in the brain, particularly in the hypothalamus, Semaglutide reduces appetite and cravings. This central effect diminishes hunger and leads to a decrease in calorie consumption.
- Impact on Weight Loss: The combined effects of reduced appetite, slower gastric emptying, and improved metabolic control contribute to substantial and sustainable weight loss for many individuals, even those without diabetes.
Approved Uses and Efficacy
Semaglutide is approved for:
- Type 2 Diabetes: To improve blood sugar control in adults, often in conjunction with diet and exercise. It also reduces the risk of major cardiovascular events in adults with Type 2 Diabetes and established cardiovascular disease.
- Chronic Weight Management: For adults with obesity (BMI ≥ 30 kg/m²) or overweight (BMI ≥ 27 kg/m²) with at least one weight-related comorbidity (e.g., high blood pressure, high cholesterol, Type 2 Diabetes). Clinical trials have demonstrated impressive average weight loss percentages, often exceeding 15% of initial body weight over a period of months.
Common Side Effects
While generally well-tolerated, Semaglutide can cause side effects, primarily gastrointestinal:
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Abdominal pain
These side effects are often mild to moderate and tend to decrease over time as the body adjusts to the medication, especially when the dose is increased gradually. Less common but more serious side effects can include pancreatitis, gallbladder problems, and thyroid tumors (in animal studies). This underscores the absolute necessity of medical supervision when using Semaglutide.
Delving into the Ketogenic Diet: A Metabolic Shift
The Ketogenic Diet, often referred to simply as "Keto," is a very low-carbohydrate, high-fat, and adequate-protein eating plan. Its primary goal is to shift the body’s metabolism from burning glucose (sugar) for energy to burning fat, a state known as nutritional ketosis.
Mechanism of Action: How the Keto Diet Works
- Carbohydrate Restriction: By severely limiting carbohydrate intake (typically to 20-50 grams per day), the body is deprived of its primary fuel source – glucose.
- Fat Adaptation and Ketone Production: With insufficient glucose, the liver begins to break down fat into molecules called ketones (beta-hydroxybutyrate, acetoacetate, and acetone). These ketones then become the body’s main energy source, fueling the brain, muscles, and other organs. This metabolic state is called ketosis.
- Impact on Blood Sugar and Insulin: The drastic reduction in carbohydrate intake directly leads to lower blood glucose levels and, consequently, lower insulin levels. This can significantly improve insulin sensitivity and is highly beneficial for individuals with insulin resistance or Type 2 Diabetes.
- Appetite Regulation: Ketones themselves, along with the high fat content of the diet, can have an appetite-suppressing effect. Many individuals on a Keto Diet report reduced hunger and increased satiety, which naturally leads to decreased calorie intake and weight loss.
Potential Benefits of the Keto Diet
- Weight Loss: The combination of reduced appetite, increased fat burning, and lower insulin levels makes the Keto Diet a highly effective strategy for weight loss.
- Blood Sugar Control: It can profoundly improve blood glucose levels and reduce the need for diabetes medications in individuals with Type 2 Diabetes.
- Improved Insulin Sensitivity: By keeping insulin levels low, the Keto Diet can help reverse insulin resistance.
- Neurological Benefits: Historically, the Keto Diet has been used to manage epilepsy and is being researched for other neurological conditions like Alzheimer’s and Parkinson’s disease.
- Reduced Cravings: Many find that carbohydrate cravings diminish significantly once in ketosis.
Potential Challenges and Side Effects
The Keto Diet is not without its challenges and potential side effects:
- Keto Flu: In the initial days, symptoms like headache, fatigue, irritability, nausea, and difficulty concentrating can occur as the body adapts to burning fat. This is often due to electrolyte imbalances.
- Electrolyte Imbalances: Low-carb diets can lead to increased excretion of electrolytes (sodium, potassium, magnesium), necessitating careful supplementation.
- Nutrient Deficiencies: Without careful planning, restricting entire food groups can lead to deficiencies in vitamins and minerals.
- Digestive Issues: Some people experience constipation due to reduced fiber intake.
- Long-term Sustainability: Adhering to such a restrictive diet can be challenging for many over the long term.
- Potential for Gallstones or Kidney Stones: In some susceptible individuals.
Who is it for?
The Keto Diet is often adopted by individuals seeking rapid weight loss, improved blood sugar control for Type 2 Diabetes, or those looking to explore its therapeutic benefits under medical guidance. It requires commitment and careful attention to food choices and nutrient intake.
The Intersection: Semaglutide and Keto Diet – A Powerful Combination?
Given the individual strengths of Semaglutide and the Keto Diet in promoting weight loss and improving blood sugar control, it’s natural to consider their combined potential. On paper, the synergy seems compelling, but the reality is more nuanced, demanding careful consideration and medical oversight.
Potential Synergies: Why the Combination Might Be Appealing
- Additive Appetite Suppression: Both Semaglutide and the Keto Diet are known for their significant ability to reduce hunger and increase satiety. Combining them could lead to an even more pronounced reduction in appetite, making it easier to adhere to a calorie deficit and achieve weight loss.
- Enhanced Blood Sugar Control: Both strategies independently lower blood glucose levels and improve insulin sensitivity. For individuals with Type 2 Diabetes, this combination could offer superior glycemic control, potentially reducing the need for other diabetes medications.
- Accelerated Weight Loss: The combined effects of profound appetite suppression, increased fat burning (from ketosis), and improved metabolic efficiency could lead to more rapid and substantial weight loss compared to either strategy alone.
- Improved Metabolic Markers: Beyond weight, the synergy could lead to further improvements in other metabolic markers such as triglycerides, HDL cholesterol, and blood pressure, contributing to overall metabolic health.
- Reduced Food Noise: Many users of Semaglutide report a significant reduction in "food noise" – the constant thoughts about food and cravings. The Keto Diet, by stabilizing blood sugar and promoting satiety, can also reduce cravings. Together, this might create a more peaceful relationship with food.
Potential Challenges and Critical Considerations
While the potential benefits are attractive, combining Semaglutide and the Keto Diet introduces several critical challenges that necessitate professional medical guidance:
- Gastrointestinal Overlap and Exacerbation: Both Semaglutide and the Keto Diet can cause gastrointestinal side effects (nausea, vomiting, diarrhea, constipation). Combining them could potentially exacerbate these issues, making the experience extremely uncomfortable and difficult to sustain. Severe nausea or vomiting could lead to dehydration and electrolyte imbalances, which are already a concern on a Keto Diet.
- Increased Risk of Hypoglycemia: For individuals with Type 2 Diabetes, especially those also taking insulin or sulfonylureas, the combination of two powerful blood-sugar-lowering interventions (Semaglutide and Keto Diet) significantly increases the risk of hypoglycemia ( dangerously low blood sugar). Close monitoring and medication adjustments by a physician are absolutely essential.
- Electrolyte Imbalances and Dehydration: The Keto Diet inherently carries a risk of electrolyte imbalances due to increased fluid and electrolyte excretion. If Semaglutide causes significant nausea, vomiting, or diarrhea, it can further deplete electrolytes and lead to severe dehydration. This could result in symptoms like dizziness, fatigue, heart palpitations, and even cardiac arrhythmias.
- Nutrient Deficiencies: While a well-planned Keto Diet can be nutritionally adequate, it requires careful attention. Combining it with a medication that can reduce appetite so significantly might make it harder to consume enough nutrient-dense foods, increasing the risk of deficiencies.
- Medication Adjustments: For individuals with Type 2 Diabetes, the need for insulin or other glucose-lowering medications will almost certainly decrease dramatically. A healthcare provider must carefully manage and adjust these medications to prevent hypoglycemia.
- Sustainability and Long-Term Health: Both Semaglutide and the Keto Diet are potent interventions. Combining them might be very effective in the short term, but the question of long-term sustainability and adherence is crucial. Maintaining such a strict regimen, especially if side effects are persistent, can be mentally and physically taxing.
- Interaction with Existing Conditions: Individuals with certain pre-existing conditions (e.g., pancreatitis, severe gastroparesis, kidney disease, gallbladder issues) may find this combination particularly challenging or even dangerous.
Navigating the Journey: Practical Advice for Combining Semaglutide and Keto
For those considering this powerful combination, a structured and medically supervised approach is paramount. This is not a strategy to undertake independently.
- Crucial First Step: Consult Your Healthcare Provider. This cannot be stressed enough. Your doctor, preferably one experienced in both diabetes management and weight loss, needs to assess your overall health, current medications, potential risks, and monitor your progress closely. A registered dietitian with expertise in ketogenic diets can also be an invaluable part of your team.
- Gradual Implementation is Key: Do not start both at once. If you are already on Semaglutide, slowly transition into the Keto Diet. If you are already on a Keto Diet, introduce Semaglutide gradually under your doctor’s supervision, especially during the initial titration phase. This allows your body to adapt to one change before introducing another, potentially reducing the severity of side effects.
- Relentless Monitoring:
- Blood Glucose: For diabetics, frequent blood glucose monitoring is non-negotiable to prevent hypoglycemia and guide medication adjustments.
- Ketone Levels: Monitor ketone levels (via blood, urine, or breath) to ensure you are consistently in nutritional ketosis.
- Weight and Body Composition: Track progress beyond just the scale.
- Symptoms: Keep a detailed log of any side effects, especially gastrointestinal issues, and report them to your doctor.
- Electrolyte Balance: Regular blood tests may be needed to monitor electrolytes, particularly sodium, potassium, and magnesium.
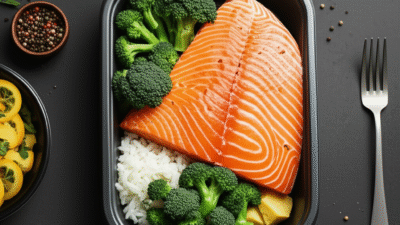
- Prioritize Quality Nutrition within Keto: Focus on a "clean keto" approach. Emphasize whole, unprocessed foods:
- Healthy fats: Avocados, olive oil, coconut oil, nuts, seeds, fatty fish.
- Quality protein: Grass-fed meats, poultry, eggs, fish.
- Low-carb vegetables: Leafy greens, broccoli, cauliflower, zucchini, asparagus.
- Avoid highly processed keto-friendly snacks or artificial sweeteners, which can sometimes trigger cravings or digestive upset.
- Vigilant Hydration and Electrolyte Management: This is absolutely critical. Drink plenty of water throughout the day. Supplement with electrolytes (sodium, potassium, magnesium) as recommended by your healthcare provider or dietitian. Bone broth can also be a good source of sodium and other minerals.
- Listen to Your Body and Communicate: Pay close attention to how you feel. If side effects are severe or persistent, or if you experience symptoms of hypoglycemia or dehydration, contact your doctor immediately. Do not try to push through significant discomfort without medical advice.
- Regular Medical Check-ups: Schedule frequent follow-up appointments with your doctor to review your progress, adjust medication dosages (especially for diabetes), and address any concerns.
- Consider a "Modified Keto" or Cyclical Approach: For some, a very strict Keto Diet might be too challenging long-term, especially when combined with Semaglutide’s effects. Discuss with your doctor or dietitian if a slightly less restrictive low-carb approach or cyclical ketosis might be more sustainable while still achieving benefits.
Who Might Benefit Most (and Who Should Be Cautious)?
Potential Beneficiaries:
- Individuals with significant obesity and Type 2 Diabetes: The combination could offer a powerful strategy for aggressive weight loss and profound improvement in blood sugar control, potentially leading to remission of diabetes in some cases.
- Those with severe insulin resistance: The combined effect on insulin sensitivity could be highly beneficial.
- Individuals who struggle with persistent hunger and cravings: The dual appetite-suppressing effects could be a game-changer for these individuals.
- Patients under strict medical supervision: This combination is best suited for those who have consistent access to and are willing to work closely with their healthcare team.
Who Should Be Cautious or Avoid This Combination:
- Individuals prone to severe GI issues: If you already have a sensitive stomach or conditions like IBS, the combined GI side effects could be intolerable.
- Those on multiple diabetes medications: The risk of hypoglycemia is much higher and requires extremely careful management.
- People with a history of pancreatitis or gallbladder disease: Both interventions can sometimes impact these organs.
- Pregnant or breastfeeding individuals: Semaglutide is not recommended, and the Keto Diet’s safety in these populations is not fully established.
- Individuals with kidney disease: The high protein intake sometimes associated with keto needs careful monitoring in kidney patients.
- Those with a history of eating disorders: The restrictive nature of keto and the appetite suppression of Semaglutide could be problematic.
- Anyone unwilling or unable to commit to rigorous medical monitoring.
Beyond the Hype: Setting Realistic Expectations and Sustainable Strategies
While the idea of combining Semaglutide and the Keto Diet for rapid and dramatic results is enticing, it’s crucial to temper enthusiasm with realistic expectations. Neither Semaglutide nor the Keto Diet, nor their combination, is a magic bullet. They are powerful tools that work best as part of a comprehensive lifestyle change.
- Focus on Holistic Health: The goal should be overall health improvement, not just weight loss. This includes improvements in blood markers, energy levels, sleep quality, and mental well-being.
- Embrace Lifestyle Changes: Medication and diet are foundational, but physical activity, adequate sleep, and stress management are equally vital for long-term success and metabolic health.
- Long-Term Sustainability: Consider how you will maintain your results once you reach your goals. Both Semaglutide and the Keto Diet are often most effective when continued. If you plan to transition off Semaglutide or relax your Keto Diet, a clear strategy for maintaining weight loss and metabolic health, developed with your healthcare team, is essential. This might involve a gradual increase in carbohydrates or continued focus on whole, unprocessed foods.
- Psychological Impact: Significant weight loss and dietary changes can have a profound psychological impact. Support from healthcare professionals, family, or support groups can be invaluable.
The Role of Your Healthcare Team: A Partnership for Success
Embarking on a journey that combines a powerful medication like Semaglutide with a restrictive dietary approach like the Keto Diet is a serious undertaking. It necessitates a strong partnership with a dedicated healthcare team.
- Your Primary Care Physician/Endocrinologist: They will prescribe and manage your Semaglutide, monitor your overall health, adjust other medications (especially for diabetes), and guide you through potential side effects.
- Registered Dietitian (RDN): An RDN with expertise in ketogenic diets can help you plan nutritionally adequate meals, address potential deficiencies, manage electrolytes, and ensure the diet is sustainable and safe for your specific needs.
- Other Specialists: Depending on your health profile, you might also consult a cardiologist, nephrologist, or mental health professional.
This team approach ensures a personalized, safe, and effective strategy tailored to your individual health status, goals, and challenges.
Conclusion
The combination of Semaglutide and the Ketogenic Diet holds significant promise for individuals seeking profound weight loss and dramatic improvements in blood sugar control, particularly those struggling with Type 2 Diabetes and obesity. Their individual mechanisms of appetite suppression, metabolic regulation, and fat burning appear to be highly complementary.
However, this powerful synergy comes with a unique set of challenges, predominantly related to the potential for exacerbated gastrointestinal side effects, increased risk of hypoglycemia, and the critical need for meticulous electrolyte management. The restrictive nature of the Keto Diet, combined with the appetite-suppressing effects of Semaglutide, demands careful nutritional planning to prevent deficiencies and ensure long-term sustainability.
Ultimately, this advanced strategy is not a do-it-yourself endeavor. It absolutely requires the close guidance and continuous monitoring of a qualified healthcare professional, ideally a multidisciplinary team including a doctor and a registered dietitian. With the right medical supervision, diligent monitoring, and a commitment to understanding and responding to your body’s signals, combining Semaglutide and the Keto Diet can be a transformative path towards achieving significant and sustainable health improvements. For the right individual, under the right care, this combination could unlock new levels of metabolic health and weight loss success.
Always consult your physician before making significant dietary or medication changes.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional before making any decisions about your health or treatment. The information provided is based on general medical knowledge and may not apply to your specific circumstances.